Vaccine Preventable Diseases

 Introduction
Introduction
All of us want to stay well and enjoy life. This is more possible today than it was 100 years ago.
In the past infectious diseases caused great fear. At a time when there was no health care system, limited scientific knowledge and equipment, no vaccinations, or antibiotics, becoming infected with a disease usually resulted in death. Infections like pertussis (whooping cough) and diphtheria, caused distressing symptoms, high rates of illness and disability. There was limited understanding of how to prevent the diseases spreading between people and causing illness.
History shows that following years of research, scientists have a better understanding of diseases and how to reduce the impact they have on people and their lives. There are now systems and processes for surveillance of diseases and interventions have been developed that can prevent deaths. Some, but not all, infectious diseases can be prevented by a vaccination.
“Vaccines have saved more human lives than any other medical intervention in history”. 1
The United Kingdom (UK) has used vaccines since the 1940s, as one of the ways to prevent diseases infecting the population. Since the establishment of the National Health Service (NHS) in 1948 a national vaccination programme of different vaccines, to be delivered across the life course has been developed. The number of notified cases of infectious diseases and related deaths has, over the years, reduced because of the programme.
For the people of Derbyshire who are vaccinated this means they are protected and can live alongside certain diseases without becoming unwell. This results in them attending their GP surgery less and avoids the need for other treatments such as antibiotics to fight secondary bacterial infections, or admission to hospital.
This overview will look at our understanding of disease, the development of vaccines, the importance of the UK national vaccination programme and how vaccines help in the control of outbreaks.
 Why is it important to Population Health?
Why is it important to Population Health?
Infectious Diseases
Actions taken to protect people from diseases, can be identified throughout history and around the world.
The Public Health Act of 1848 was introduced after Victorian England experienced multiple outbreaks of diseases, due to the growing population living in overcrowded houses and slums with insanitary conditions. Subsequent years bought better understanding of how infectious diseases were spread. This challenged centuries of thinking that foul air, or vapour, was thought to be the source of diseases. It took multiple cholera outbreaks before there was acceptance of theory from John Snow that cholera was a water-borne infection. This is the foundation of the public health work which continues today.2,3
Diseases are usually identified when we become unwell with certain symptoms. We may have samples taken, such as blood, saliva, or a small amount of body tissue. These samples will go to the laboratory for testing which will help diagnose or rule out various diseases.
The UK has developed a notification system for certain diseases. Once notified to the authorities they can be investigated and actions to be taken to prevent spread to others such as isolating the source e.g. food, water, or people. If action isn’t taken, large numbers of people can become unwell. This can cause healthcare systems to be overwhelmed, and people are unable to receive the care they need. There can also be repercussions across wider society with business and other services being impacted.
Research has helped our understanding of diseases and led to the best protective measures being introduced such as clean drinking water, standards for food hygiene, waste disposal, hand hygiene and vaccination.
Vaccinating people as a way of developing protection (immunity) from some diseases, has developed over many years. It is a technique used all over the world. Not all infectious diseases can be prevented by vaccines and so it is necessary to adopt a range of measures to prevent the spread of germs, to keep the population healthy and well.
Vaccines
The theory of vaccination originated in India and China. During the 18th century these ideas were taken up by scientists in the western world. Edward Jenner’s work controlled the spread of smallpox and Louis Pasteur’s work influenced vaccine development. Modern vaccine technologies of the 21st century continues to build on this the early pioneering research and has led to the introduction of many new vaccines against specific infections. These vaccines have kept the population safe and reduced the number of deaths and disease.4,5
The words vaccination and immunisation often get used as though they are the same thing, they are not. Vaccination is the giving of the vaccine, whereas immunisation is the process that happens in our bodies after we have had the vaccine, to develop the protection needed.
Vaccines are developed to protect us from specific diseases. The flu vaccine will protect us from serious flu infection, the Pertussis (whooping cough) vaccines protect us from serious whopping cough infection. Therefore, it is important to have all the vaccines that are available to you on the national vaccination programme.
The development and establishment of the UK’s recommended programme of vaccination, means diseases that were previously common are now less so. Because of this, some believe the diseases have gone away and no longer pose a risk to their health. This is not the case; diseases continue to circulate in our environment and cause illness. We know this because vaccine preventable infections such as measles and whooping cough are reported regularly to United Kingdom Health Security Agency (UKHSA). However, the numbers are much fewer than in the early years of the NHS, because of the protection that the current vaccination programme provides.
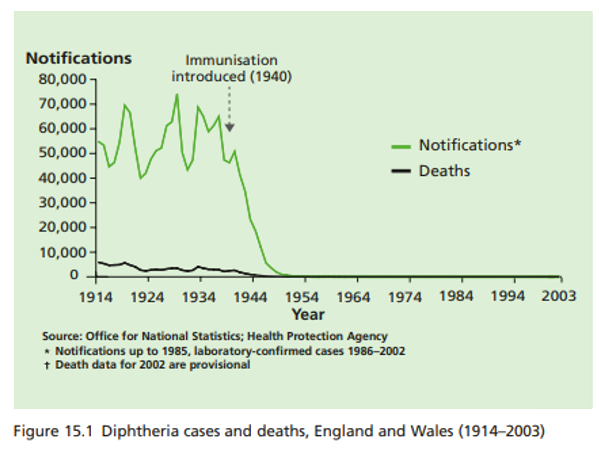
In the 1940’s, diphtheria was a common disease in the UK. It is a bacterial infection which can cause respiratory symptoms which are distressing to both experience and see. Symptoms range from a sore throat, fever and to developing a thick film “membrane” which covers our airways that we need use to breathe. Death can be by suffocation caused by breathing in the developed membrane. Prior to the 1940’s more than 61,000 people were infected in the UK, of which 3,283 died.6,7
The graph below “Diphtheria cases and deaths England and Wales 1914 – 2003” shows, after the population are given the new diphtheria vaccination, across the 1940’s the numbers of people suffering with illness and dying as a result of diphtheria infection reduced dramatically.8
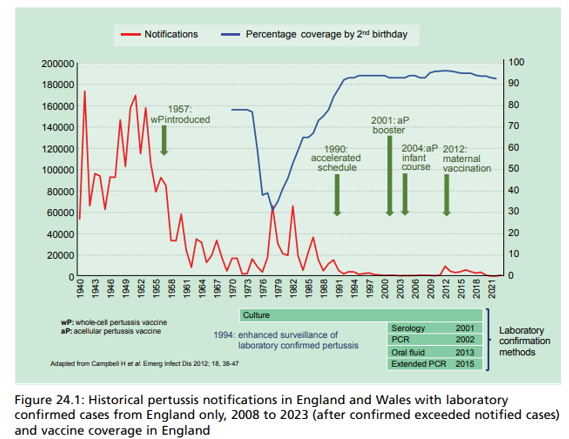
Whooping cough was a common infection in the 1950’s. Called whooping cough because it causes us to cough, violently and rapidly, until all the air has left our lungs and we are forced to inhale, causing a “whooping” sound. It affects all age groups. The irritating cough can become uncontrollable, and we may vomit as a result. The cough can last for up to three months.
Our lips and tongue may turn blue during coughing spells, because we are unable to take in sufficient oxygen. The symptoms are distressing to both experience and observe in others. Severe complications and deaths occur most commonly in unvaccinated babies less than six months old.
In response to an increase in infant cases and deaths due to whooping cough during 2011, a whooping cough vaccination programme was introduced for pregnant women. This allowed babies to obtain whooping cough antibodies (a substance that can fight the disease) from their mother before birth. Babies would then be protected from birth until they were old enough to be protected by the routine infant vaccination programme.
Following the introduction of the specific whooping cough vaccination programme for pregnant women, the number of deaths in babies reduced. Today the whooping cough vaccine is now established as one of the vaccines offered to pregnant women.
The graph below shows since its introduction in 1940’s the whooping cough vaccine has been improved, and the programme of delivery adapted, to keep the most vulnerable protected and the numbers of whooping cough cases and deaths low.9
 The Derbyshire Population Health Approach
The Derbyshire Population Health Approach
The Derbyshire Population Health Approach focuses on prevention, population health, evidence-informed practices, causes, and collaboration. It emphasises proactive measures to prevent health issues, tailors interventions to specific populations, incorporates evidence-informed practices, addresses underlying causes, and promotes collaboration for effective action.
When considering the topic of vaccine preventable diseases within The Derbyshire Population Health Approach:
• Prevention
In the UK, we are now offered vaccines throughout our lives, not just childhood. Certain features of our lives - growing up, having a baby, travel (in and out of the UK), the job we have, changes in our medical condition and, growing old, mean we could be exposure to certain germs and at risk of becoming unwell.
The aim of the vaccination programme is to ensure we receive appropriate vaccines to allow us to develop protection (immunity), before we are exposed to particular germs.
The UK has a free national vaccination programme.
It includes -
- routine immunisation schedule (different vaccines offered throughout our life course
- Selective immunisation programmes that target children and adults (including pregnant women) at particular risk of serious complications from certain germs,
- Additional vaccines for individuals with underlying medical conditions10
Where can the people of Derbyshire have their vaccinations?
The majority of the vaccines in the routine immunisation schedule are offered and delivered by staff in a GP surgery. When we become eligible for vaccines from the schedule, we will be invited to make an appointment with the practice nurse, so the vaccine can be given. We need to be registered at a GP surgery for this to happen.
Local pharmacists are able to deliver a few specific vaccines such as flu and COVID 19. Appointments can usually be made online with the relevant pharmacy.
There are specific services provided in Derby and Derbyshire hospital maternity services, delivering vaccinations to pregnant women. Some of these vaccines are offered to protect the woman whilst she is pregnant. Other are given to protect the baby.
There are specific services provided in Derby and Derbyshire schools, delivering vaccinations to children of school age. These vaccines are offered as part of the school age immunisation service (SAIS), which is only available in schools or clinics run by SAIS. The vaccines delivered by SAIS cannot be given at GP surgery.
• Population
Across the Population
Diseases are always present in the environment. They are easily spread across the population because people have contact with the environment and, each other.
If we are unvaccinated, there is a risk we will come into contact with diseases and, how our bodies will respond to certain diseases is uncertain. If we are exposed to a disease we are not vaccinated against, evidence shows there is a risk we may become ill, possibly need hospital care and may develop medical problems e.g. a chest infection, as our body’s immune system fights the disease. We could be ill for a number of weeks. Some of us, regardless of our age, will die as a result of being infected.
After being infected, we may develop some protection against re-infection. However, it is uncertain how much protection we will have, and this means we are at risk of being re-infected.
The advantage of having vaccines before we are exposed to a disease reduces those risks. Being vaccinated ensures sufficient protection from severe illness, without causing the illness and risk of known medical complications. The days following a vaccination, we may experience a fever, aches or headaches, this is our body responding as if it is preventing an infection. This is expected, a normal part of the immune response and shows the vaccine is working. Evidence shows these expected side effects will resolve in a few days.
Vaccines are effective in protecting us from serious illness, however they are not 100% effective at preventing infection so we may still experience mild symptoms if we are exposed to the specific disease.
Reasons to be vaccinated -
To stop the spread of diseases -If we become ill, our children, grandchildren, and parents may also be at risk of becoming ill. Having all recommended vaccines makes it less likely we will spread germs from person to person.
To protect the most vulnerable - If most of us are vaccinated and immune to diseases, others who cannot receive a vaccine can also be offered some protection. High numbers of people being immune creates ‘community immunity’. The diseases run out of a place to live and grow, and it’s opportunity to spread is reduced.
To stay connected - illness from an infection can result in lost time and money from work, lost time from education, from family and from the things we enjoy. We may not be able to care for those who depend on us, because of illness.
To protect themselves from circulating infections –certain viruses and bacteria circulate around us. If we are vaccinated and have developed immunity against certain diseases and infections, we are protected from serious illness. If we are unvaccinated and therefore, unprotected, we remain at risk of infection and the complications that may bring.
Vaccines are designed to prevent disease, not cause it – vaccines are not made to pass on disease, as they contain either killed or weakened parts of a disease, which is sufficient for the body to be able to respond to.
Vaccines are safe
The UK has the Medicines and Healthcare products Regulatory Agency (MHRA) in place to ensure that all licensed and approved vaccines are safe. Potential side effects associated with vaccines are uncommon and much less severe than the diseases they prevent.11

Vaccines
The way vaccines are developed has evolved over time with the application of knowledge and research.12
“Platform technology” now plays a major role providing a foundation template for future vaccines to be built upon. The template contains knowledge of the basics, such as manufacturing technique sand storage requirements etc. This platform of knowledge reduces future development time and costs. More importantly if a new vaccine is needed quickly, such as during a pandemic, there is a template to work from avoiding the need to start from nothing.
Vaccine vs the Virus: This race, and the next one. Sarah Gilbert 44th Richard Dimbleby lecture transcript.13
The patient information leafletsincluded with the vaccine, provides helpful information including a list of the contents of the vaccine. In addition to a few drops of water, they need to contain active products such as an antigen, which is a substance that causes the body to make protective cells.
The information leaflet may also show substances used to manufacture the vaccine but not added to the vaccines. They may be present in trace amounts in the final product.
Across the world, vaccines are continually researched, designed, developed, licenced, and monitored.14
In the UK before a new vaccine can be used, there are three different phases of clinical trials that must be completed. The trial data is reviewed by the UK government Medicines and Healthcare products Regulatory Agency (MHRA) to ensure this new product meets safety, quality, and effectiveness standards before licences are given allowing manufacture and use. Once in use the vaccines are monitored via Yellow Card Reporting.15
Yellow Card Reporting relies on voluntary reporting of suspected side effects by health professionals and the public. This openness means that reported events are not always proven as side effects caused by the vaccine. However, the reporting provides an early warning that the safety of a vaccine may require further investigation. It is important for people to report problems experienced with any medicines as they may identify issues not previously known about.
Vaccines have some commonly known side effects, such as a sore arm, redness etc. these effects pass in a couple of days and may not affect everyone. More serious side effects are referred to as adverse reactions.16
Some reactions may not be related to the administration of a vaccine, they may have happened anyway, regardless of having a vaccination - particularly when millions of people are vaccinated, and especially when vaccines are being given to the most elderly people and those with underlying illness.
What are vaccines?
Vaccines are usually in liquid formulation and are given either by an injection, nasal spray or drops in the mouth.
Unlike other medicines, vaccines are given to us when we are well, to allow us to build protection from diseases in a controlled way. They are formulated to give our immune system the memory of what a particular disease looks like, sometimes only exposing us to part of a disease, in order for this to happen. Once vaccinated it takes the body approximately two weeks to develop full immunity, so it is important to ensure we avoid being exposed to diseases during that time.
Once a high number of the population is vaccinated against a particular disease, it is hard for the diseases to spread. This is because the number of people who could have been infected, has been reduced by the use of vaccines.
Those people that cannot be vaccinated, such as very young infants and people receiving chemotherapy, will be protected if vaccine uptake is high. Diseases will always circulate, it is due to being appropriately vaccinated, that protects from becoming seriously unwell.17,18
• Causes
Vaccines have been used across the world, for many years. They are administered to the population to keep them safe from severe illness and death, caused by certain diseases
For vaccines to benefit everyone, the majority of the population need to be vaccinated. If the numbers of people being vaccinated reduces, this allows the diseases to find hosts and results in an increase in cases of illness and disease.
Over the last 15 years,
- the number of vaccines offered across the course of our life has increased.
- The availability of vaccine related information has grown.
- Settings where vaccines are delivered has changed - vaccines are now administered by a variety of professionals in a range of different settings, such as general practices, schools, prisons, care homes or a high street pharmacy.
- research has shown the majority of the population are motivated to be vaccinated.
A Recent UKHSA report (2025) Quality criteria for an effective immunisation programme states however, “there has been a gradual year on year decline in uptake for the routine childhood immunisation programme since 2013”.19
• Collaboration
To address the decline in vaccine uptake system partners, who are involved in the delivery of the vaccination programmes to the population, work together at all levels.
It is essential everyone can access vaccines, to ensure we all have our health protected and, diseases do not spread between us.
Local organisations must ensure services are delivered in a way that suits the population. Efforts should be made to understand people’s preferences and incorporate them into service delivery. There must also be reference to studies which consider vaccine uptake and relevant recommendations utilised.
Recent studies from Royal College of Paediatrics and Child Health and the UK Health Security Agency have recommended the key factors for local partners consider are -
- Simple booking systems
- Flexible appointment arrangements
- Venues appropriate for intended attendees
- Well trained workforce
- Accessible trusted health and vaccine information in a variety of formats.
- Good supply of vaccines
In order to seek views on vaccination services from Derbyshire people, Derbyshire Public Health team engage with the community voluntary sector, who have very strong links with local groups and settings. Using these links, they can organise focus groups or carry out commissioned surveys.
Public health staff also run engagement sessions with members of the public in various settings. This provides opportunities to seek their opinions of vaccination services and gain an understanding of the matters they raise. Those communities found to be underserved by the current system of vaccination services are also consulted, as it is of primary importance
to ensure their views are heard when vaccination services are being planned.
Providers of vaccination services are consulted to ensure any issues with the service delivery are identified and solutions sought.
Networking conversations across the country help identify and share learning, in order to improve vaccine uptake.
 Latest Derbyshire Data
Latest Derbyshire Data
Trend Data
Derbyshire Quilt
Prevalence Maps of Derbyshire
The maps below illustrate various geographies for Derbyshire. LSOAs and MSOAs are geographical divisions used for statistical purposes, allowing for more detailed analysis of local data. In these maps, you can explore various health indicators and data for Derbyshire, providing valuable insights into the area’s health and wellbeing.
Wards Data Not Available
Data for this geography is not yet available. Please check back later.
Districts Data Not Available
Data for this geography is not yet available. Please check back later.
 |
In the top right of the map, you’ll find the ‘Layer Control’ icon. This is an easy way to customise what you see on the map visualisation. Click the ‘Layer Control’ to choose which information is displayed on the map. Pick the indicator that interests you the most, and the map will transform accordingly. |
Slope Index
This chart illustrates the differences in health and lifestyle factors across areas in Derbyshire, from the most deprived (decile 1, red) to the least deprived (decile 10, green). As you move from left to right on the chart (from more deprived to less deprived areas), the line shows whether these factors are becoming more or less common. Essentially, it’s a way to see how living in wealthier or poorer areas affects the prevalence of these factors.
 Further Analysis & Assessments
Further Analysis & Assessments
Derbyshire Joint Strategic Needs Assessment (JSNA) involves a thorough examination of a specific health problem, exploring its causes, consequences, and underlying factors. It combines various data sources, collaboration with stakeholders, and rigorous analysis to generate insights for evidence-informed interventions and policy changes.
 More Information & Resources
More Information & Resources
Here is a list of useful resources and information to help prevent issues related to domestic abuse. These materials are meant to provide individuals, healthcare professionals, and communities with the knowledge and tools they need as part of efforts to address domestic abuse-related harm.
Contributors
Linda Drew, Advanced Public Health Practitioner, Health Protection
Footnotes
Wilson J (2000) 8th edition Clinical Microbiology - an introduction for healthcare professionals Bailliere Tindall↩︎
The history of immunisation | Association of Directors of Public Health↩︎
Vaccine-preventable diseases | European Centre for Disease Prevention and Control↩︎
Diphtheria Disease Information | European Centre for Disease Prevention and Control↩︎
The complete routine immunisation schedule, September 2025 | UK Health Security Agency↩︎
Benefits of vaccination | European Vaccination Information Portal↩︎
How vaccines are researched and developed | The Association of the British Pharmaceutical Industry↩︎
Vaccines vs the Virus: This race, and the next one: Sarah Gilbert 44th Richard Dimbleby lecture transcript | University of Oxford↩︎
Yellow Card reporting site | Medicines & Healthcare products Regulatory Agency↩︎
How vaccines are tested, licensed and monitored | Vaccine knowledge | University of Oxford↩︎
Vaccine-preventable diseases | European Centre for Disease Prevention and Control↩︎
The history of immunisation | Association of Directors of Public Health↩︎
Quality criteria for an effective immunisation programme | UK Health Security Agency↩︎