Influenza

 Introduction
Introduction
Influenza (flu) is an acute viral respiratory illness which can easily spread between people, symptoms include a high temperature, body aches, headache and feeling exhausted.
There are three types of influenza viruses which affect humans (A, B and C) with types A and B responsible for most of the flu infections. The flu virus is constantly changing and the World Health Organisation (WHO) assess which flu strains should be included in the seasonal vaccine to ensure the best protection.
Flu can range from being manageable at home to hospitalisation and death. The average number of deaths from flu in England is 13,500.1
Some people are more vulnerable to the effects of flu and it can make them more ill, increase the risk of complications or worsen symptoms of existing conditions. Flu can be spread between individuals even with mild or no symptoms.
People often say they have ‘had flu’ when they have had a bad cold – the difference between a cold is that a cold appears more gradually than flu which can appear within a few hours. A cold mainly affects your nose and throat and you are able to generally carry on with your usual day to day activities whilst feeling unwell. Flu can make you exhausted so that you are unable to carry on as normal and need to fully rest and recover.
There is a seasonal influenza (flu) vaccine which is available free to those who are at most at risk of becoming seriously ill.
 Why is it important to Population Health?
Why is it important to Population Health?
Flu is important to population health for many reasons:
Flu affects individuals health but also has an impact on the health and social care system and workplaces. This includes increased General Practititioners (GP) consultations, hospital admissions, delays to discharge and care home closures. This all adds pressure onto the health and social care system.
Every winter people become ill with flu. While some people are able to recover at home and need to be off work ill, others will need GP and hospital treatment. Flu often has a ‘peak’ in cases over the winter months where the greatest impact is felt on services. An individual admitted to hospital with flu is more likely to need an intensive care unit bed or high dependency unit bed. The recovery time following hospitalisation can be long and impact on working and family life.
People most at risk of serious illness from flu include children under 6 months, older people, those with underlying health conditions (including respiratory and cardiac disease, diabetes, chronic liver disease, immunosuppression) and pregnant women.
Flu can make existing conditions worse, such as asthma. Complications from flu can include a secondary bacteria infection such as pneumonia. This can lead to increased use of antibiotics which contributes to antimicrobial resistance.
Pregnant women are at increased risk of serious illness and complications from flu this can include premature birth, smaller neonatal size, lower birth rate and perinatal mortality.
Care home residents are also more likely to be seriously ill with flu and more likely to experience hospitalisation. An outbreak (2 or more cases) of flu within a care home can mean visitors are asked to stay away which has an impact on mental wellbeing of residents, family/friends and carers. An outbreak can impact on hospital discharge processes. In addition if staff are off work with flu this can impact continuity of care and familiarity whilst also putting pressure on other staff or increased cost of using agency staff.
Every winter in England an average of 13,500 people die from flu. The majority of deaths are people over 65 years, however deaths happen across all age ranges including children under the age of 4 years.2
 The Derbyshire Population Health Approach
The Derbyshire Population Health Approach
The Derbyshire Population Health Approach focuses on prevention, population health, evidence-informed practices, causes, and collaboration. It emphasises proactive measures to prevent health issues, tailors interventions to specific populations, incorporates evidence-informed practices, addresses underlying causes, and promotes collaboration for effective action.
When considering the topic of Flu within The Derbyshire Population Health Approach:
• Prevention
To avoid the spread of flu general infection prevention guidance must be followed. This includes thoroughly washing your hands at key points e.g. before eating food, after using the toilet and after blowing your nose or coughing. Ventilation is important alongside cleaning surfaces as the flu virus can live on surfaces for 24 hours. Respiratory hygiene is important particularly during the winter time, this includes with the the key message of ‘catch it, bin it, kill it’. People are most contagious in the first 5 days of having flu but good hand and respiratory hygiene should be practiced all year round.
As the flu virus that is circulating can change each year the WHO monitor this and then assess which flu strains should be included in the seasonal vaccine to ensure the best protection.
The flu vaccination is available free to the population who are most at risk of becoming seriously ill and those who care for them (healthcare workers, social care workers and carers). Some employers choose to purchase flu vaccines for their employees who are not eligible under the National Health Service (NHS) free scheme or individuals not identified as being able to have a free flu vaccine can choose to purchase a vaccine at a pharmacy.
Delivery of the flu vaccine is from a variety of providers, most are delivered via GP practices (over 65s, under 65s at risk groups and children 2/3 years), children who are school aged are able to have the influenza flu nasal spray via the School Aged Immunisation Team, pregnant women can access a vaccination either through their maternity provider or GP, care home residents are vaccinated either through a GP or pharmacist visiting their home. For health care workers and social care workers flu vaccines are available via an occupational health provider, where in place, or a GP or pharmacist.
The complexity of accessibility of a flu vaccine can make it difficult both for individuals to acquire a vaccine and to identify trends in uptake. For example a pregnant healthcare worker is eligible for a vaccine due to her pregnancy and occupation.
• Population
People most at risk of the complications of flu or a more serious illness from flu include: Children under 6 months, older people, pregnant women and those with underlying health conditions. These health conditions include respiratory and cardiac diseases as well as immunosuppression.
The uptake of flu vaccinations shows lower uptake across different georgraphic areas, including in more deprived areas and within some of the eligible cohorts. For example, uptake is lower amongst social care workers than people who are over 65 years old. When the uptake of vaccinations is lower it more likely that there will be cases of flu. This leads to impacts such as illness, time off work, hospitalisation or death.
• Evidence
Each year WHO assesses which strains of flu are likely to circulate in the northern hemisphere during winter using the relevant epidemiological data. The vaccine is developed to respond to the predicted strains. The annual flu vaccination programme was started in the late 1960s with changes to the cohorts being decided by Joint Committee on Vaccination and Immunisation (JCVI) using all available evidence. The annual childhood flu programme was introduced in 2013. The guidance for the flu vaccination programme is released each year by the Chief Medical Officer, UK Health Security Agency (UKHSA) and NHS England (NHSE).
The ‘green book’ has a chapter detailing the clinical risk groups and the guidance needed to vaccinate.3 The NHSE Vaccine strategy outlines a co-ordinated evidence based approach for a system wide approach to improving vaccine delivery including influenza.
Evidence about lower uptake in populations is growing with new reports being published regularly.

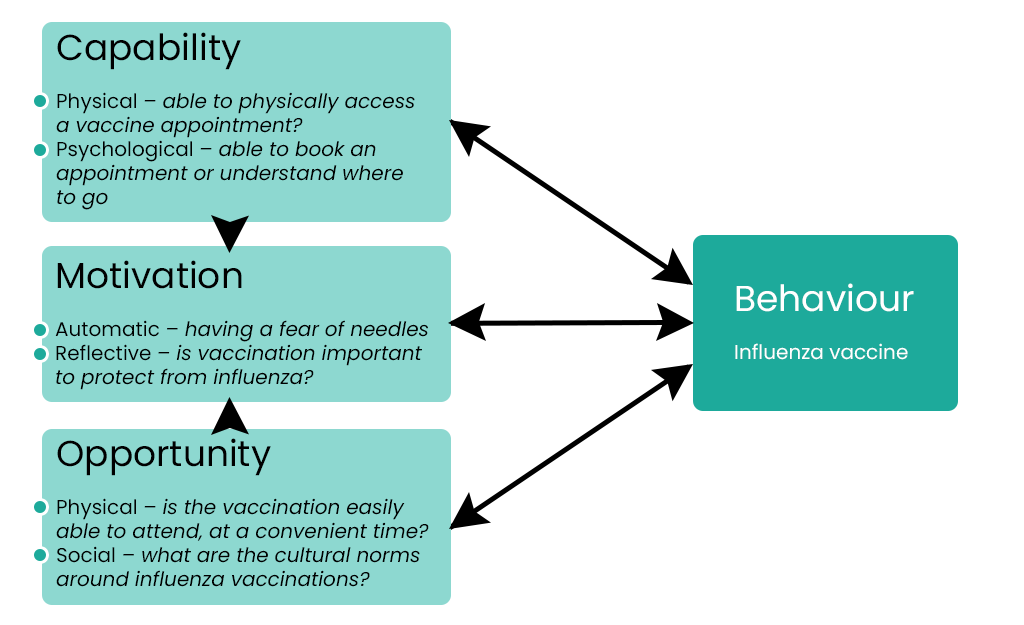
Flu is spread through germs from an infected person being transferred to someone else. This can be through coughs and sneezes or touching surfaces. Settings where people are in closer contact with each other see a higher risk of transmission of influenza. This can include places such as education and early years settings, care homes and prisons. Flu ‘season’, where there are the most cases, is also over the winter months when more people meet indoors with less ventilation. Although the flu vaccine is a safe and effective way to reduce the impact of flu there is lower uptake across several of the cohorts including pregnant women, under 65s with a long term condition and healthcare and social care workers. Lower uptake of the flu vaccine can result in higher levels of flu in the community, more hospitalisations or deaths. Some people do not have their offered vaccine due to the immune response felt afterwards (side effects), particularly if they do not want to take time off work, however conversely more work days are lost if someone has flu. The reasons behind lower uptake of influenza vaccines in the groups discussed above are complex. Some can be explored using the COM-B model (see below) which gives a rounded approach to vaccine uptake. This model would need to be applied to each community of people whose uptake is lower than others. Once this is completed actions can be put in place to help address each step of the model e.g. psychological capability – being able to book an appointment online can be supported through community initiatives to tackle digital deprivation.

Collaboration between all system partners is important to increase flu vaccine uptake. This includes the use of data and evidence to underpin decision making across the system. There should be a collaborative approach to reducing vaccine inequalities. The delivery of vaccines, whether via GP, pharmacist, maternity services, occupational health providers or the school aged immunisation service, must be equitable and fit the needs of the recipients. The wider healthcare and social care workforces should be vaccine-informed through appropriate training and information. Community collaboration is needed as part of the effort to increase uptake of all vaccines including influenza. This includes communities defined by their location, occupation or demographics. Understanding and addressing the barriers that communities face to access a influenza vaccination need to be addressed as a wider system.
 Latest Derbyshire Data
Latest Derbyshire Data
Trend Data
Derbyshire Quilt
Prevalence Maps of Derbyshire
The maps below illustrate various geographies for Derbyshire. LSOAs and MSOAs are geographical divisions used for statistical purposes, allowing for more detailed analysis of local data. In these maps, you can explore various health indicators and data for Derbyshire, providing valuable insights into the area’s health and wellbeing.
 |
In the top right of the map, you’ll find the ‘Layer Control’ icon. This is an easy way to customise what you see on the map visualisation. Click the ‘Layer Control’ to choose which information is displayed on the map. Pick the indicator that interests you the most, and the map will transform accordingly. |
Slope Index
This chart illustrates the differences in health and lifestyle factors across areas in Derbyshire, from the most deprived (decile 1, red) to the least deprived (decile 10, green). As you move from left to right on the chart (from more deprived to less deprived areas), the line shows whether these factors are becoming more or less common. Essentially, it’s a way to see how living in wealthier or poorer areas affects the prevalence of these factors.
 Further Analysis & Assessments
Further Analysis & Assessments
Derbyshire Joint Strategic Needs Assessment (JSNA) involves a thorough examination of a specific health problem, exploring its causes, consequences, and underlying factors. It combines various data sources, collaboration with stakeholders, and rigorous analysis to generate insights for evidence-informed interventions and policy changes.
 More Information & Resources
More Information & Resources
Here is a list of useful resources and information with regard to flu. These materials are meant to provide individuals, healthcare professionals, and communities with the knowledge and tools they need as part of efforts to address flu as a population health topic.
Contributors
Claire Jones, Public Health Lead, Health Protection