Bowel Cancer

 Introduction
Introduction
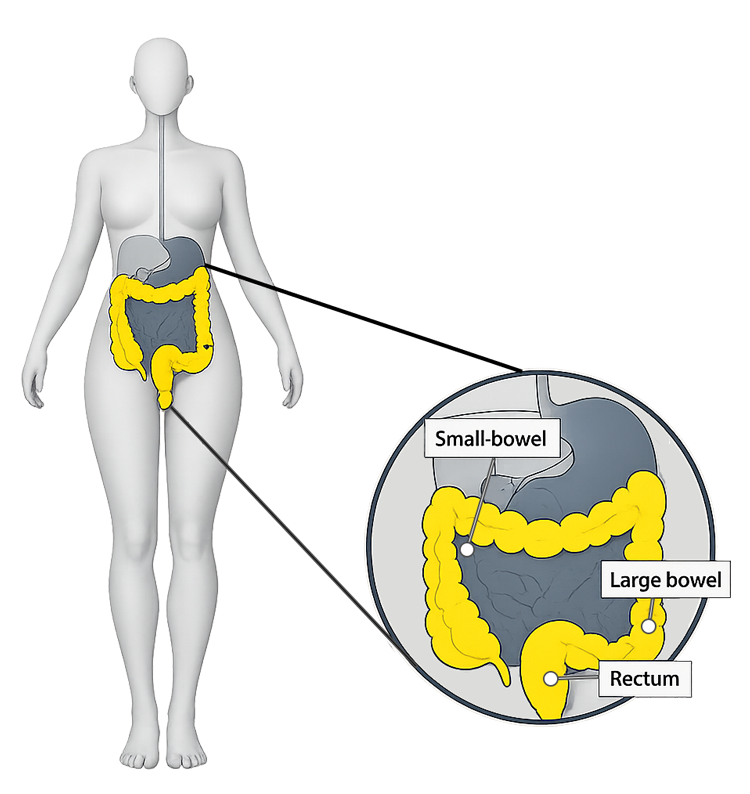
The human bowel is known or referred to in two parts, the small bowel (small intestine) and the large bowel (Colon- large intestine). The small bowel is approximately 6-8m long and 2cm wide, whilst the large bowel is approximately 2m long and 6-7cm wide.
A part of the digestive system, the bowel works to digest the foods we eat, absorbing the nutrients, and then removes the waste we cannot use.
Bowel cancer is cancer that is found to be anywhere in the large bowel, including the colon and rectum. Depending on where it is found, bowel cancer may also be called colorectal cancer, colon cancer or rectum cancer.1
Bowel cancer is the fourth most common cancer in the UK, with almost 44,000 people diagnosed in the UK every year. Bowel cancer can affect anyone of any age, however, 94% of cases are diagnosed in people over 50 years of age. Whilst more prevalent in people of 50 years, there are 2,600 new cases in people under 50 every year.2
As in most cancers, early diagnosis is key, with bowel cancer being very treatable and curable if diagnosed early.The diagnosis usually comes via two pathways: the national screening programme or the symptomatic pathway, where an individual presents to their GP with concerns.
The vast majority of bowel cancer diagnoses are from the symptomatic pathway of which symptoms can include:
- Bleeding from your bottom
- Blood in your poo
- A change in how often you poo or regularly having diarrhoea or constipation
- Losing weight, but not sure why?
- Feeling very tired all the time but not sure why?
- A pain or lump in your tummy
Screening
The NHS offers universal bowel screening every 2 years, for everyone aged between 50-74. Bowel screening involves sending a stool (poo) sample to the lab every 2 years so that it can be tested for traces of blood. The test is known as FIT (Faecal Immunochemical Test). Approximately 10% of new diagnosis are from the FIT tests. A test kit will be sent out automatically when screening is due, so it is important that contact details, including home address, are kept up-to-date on GP health records.3
The majority of screening results are normal and in this case another test kit will be sent out when screening is next due.
If blood is found using FIT, an appointment will be offered with a specialist, which is usually by telephone. The specialist will discuss the next steps of screening, which is usually a colonoscopy.
The colonoscopy is extremely important in preventing and diagnosing bowel cancer. A colonoscopy could be offered either as a result of a positive screening result (FIT test) from routine screening, or if an individual has symptoms and is referred by a GP.4
A colonoscopy is a long flexible tube that is inserted through the rectum; it has a bright light and camera to allow doctors to view the large bowel and check for any polyps or signs of cancer. Should any polyps be found, these may be removed, as a preventative measure as they could become cancerous later on. Other tests such as a CT scan may also be carried out.
There are different stages and grading of bowel cancer, referred to as the TNM system. T (Tumour) - how far has the tumour grown into the bowel wall (ranging from T1-T4), N (Nodes) - whether the cancer has spread into nearby lymph nodes (ranging from NO-N2), M (Metastases) - whether the cancer has spear (metastasized) to other parts of the body (ranging from MO-M1).
The number stages use information from the TNM system
Stage 1 - The cancer hasn’t spread outside the bowel wall
Stage 2 - The cancer has grown into or through the outer layer of the bowel wall
Stage 3 - The cancer has spread to nearby lymph nodes.
The cancer has spread to other parts of the body.
Treatment of bowel cancer will depend on a person’s individual diagnosis, general health and consider any other factors as necessary. Treatment may include, surgery, radiotherapy, chemotherapy, or a combination of each.
 Why is it important to Population Health?
Why is it important to Population Health?
Bowel cancer is important to population health due to its frequency, preventability, and the benefits of early detection. Investing in screening programmes, public awareness and lifestyle interventions can significantly reduce its impact on individuals and the healthcare system.
The government recognises the impact of bowel cancer for population health and has a national screening programme in place. Furthermore, this programme has been expanded, with the age range lowered, in recognition of early diagnosis and early treatment.
The NHS 10-year plan includes initiatives to improve access to screening, genetic testing and early diagnosis to reduce death from cancer.
Early detection
Bowel cancer is very much a treatable cancer, especially when found early. 90% of people with stage 1 bowel cancer will survive their cancer for 5 years or more after they are diagnosed, with this reducing to 10% when diagnosed at stage 4.5
Consequences
Bowel cancer is the second leading cause of death in the UK. Even after treatment, it can lead to physical symptoms such as anaemia, fatigue and bowel habit changes, which can impact overall health, well-being and ability to work.
Challenges
Bowel cancer rates are rising in the UK, especially amongst the younger population. This could be due to social and cultural changes in diet and lifestyle. Early awareness of symptoms and accessing medical care is key. Whilst there are barriers to the screening programme, such as fear of the procedure (Colonoscopy), access and social and cultural barriers continue to be supported and addressed to increase early diagnosis and treatment.
Economic impact
According to the 2020 report, ‘The cost of cancers of the digestive system in Europe’ IHE Report 2020:6, bowel cancer costs the UK economy more than £1.7 billion a year, this was calculated on diagnosis, treatment, and other associated costs of loss of income, and informal care provided from friends and family.
 The Derbyshire Population Health Approach
The Derbyshire Population Health Approach
The Derbyshire Population Health Approach focuses on prevention, population health, evidence-informed practices, causes, and collaboration. It emphasises proactive measures to prevent health issues, tailors interventions to specific populations, incorporates evidence-informed practices, addresses underlying causes, and promotes collaboration for effective action.
When considering the topic of bowel cancer within The Derbyshire Population Health Approach:
• Prevention
Bowel cancer UK report that scientists believe by having a healthier lifestyle, around half (54%) of bowel cancers could be prevented.6 This healthier lifestyle focuses on the 4 main areas of:
Diet and maintaining a healthy weight
Being overweight or obese can increase the risk of bowel cancer. Maintaining a healthy diet can not only support a healthy body weight, but also helps keep your digestive system working well, which in turn can reduce the risk of developing bowel cancer.
Physical activity
Being physically active can help reduce the risk of bowel cancer by helping maintain a healthy body weight.
Reduced alcohol use
Alcohol is linked to increasing the risk of several cancers, bowel cancer included. Alcohol increases the risk of cancer developing as it damages the cells that line the inside of the bowel.
Stopping smoking
Smoking increases the risk of developing polyps (non-cancerous growths) which could develop into cancer if not treated.
Whilst some of the bowel cancer risk factors are non-modifiable as they are linked to familial history and other diseases, there are modifiable lifestyle factors which can be positively influenced and changed such as:
- stopping smoking
- losing weight via eating a healthy diet
- stay active and exercise regularly
- reduced alcohol consumption
- and eating less red meat and processed meat
A core part of the prevention strategy for the population of Derbyshire is encouraging residents to participate in bowel screening. Nationally, the rate of screening uptake is around 70%, which is also reflected locally within Derbyshire. Work is ongoing to increase uptake further, and to better understand the barriers to screening.
• Population
The introduction of the FIT test has improved screening participation from under 60% to nearly 70%. However, there continues to be disparities, with lower screening uptake in deprived communities, minority groups, those that are non-English speaking and the learning disability community. There is a higher incidence of bowel cancer at a younger age, due to genetic factors in certain minority groups, particularly black and Asian.
In Derbyshire, the county is varied in its make-up, from highly populated areas to areas of rurality. This creates barriers of transport and access to hospitals for people undertaking a colonoscopy. The required preparation for the colonoscopy and aftercare from having sedation, pose additional challenges to people, limiting transport options, time off from work or needing the support of others.
• Evidence
Bowel cancer is the UK’s second biggest cancer killer, with fewer than 4 in 10 people diagnosed at the earliest stages. Early diagnosis and timely treatment can save lives, and through the NHS 10-year plan, the government has committed to reduce the number of lives lost to cancer through early diagnosis by:
- Making cancer screening easier to access and more targeted, by using joined-up health records that include things like genetic risk and test results.
- Giving all cancer patients the option of detailed genetic testing, including Lynch syndrome, to help guide their treatment and new blood tests that could help spot cancer earlier.
- Offering 10,000 cancer vaccines to patients in trials over the next 5 years and roll them out more widely if they prove effective.
- Test and introduce new ways of spotting cancer early, including using new technologies that can detect multiple types of cancer from a single test.7

As with most cancers, there are a range of risk factors that can influence a person’s risk of developing bowel cancer, some of them are modifiable (can be changed) such as:
- Smoking
- Overweight
- Alcohol use
Whilst the others are non-modifiable (can’t be changed):
- Being over the age of 50
- Family history (close relative had bowel cancer)
- Associated conditions such as Inflammatory bowel disease, including Crohn’s disease and ulcerative colitis
- Bowel polyps (however, smoking and obesity increase the risk of polyps)
- Lynch syndrome or familial adenomatous polyposis
Lynch syndrome (LS) which used to be called hereditary non-polyposis colorectal cancer (HNPCC), is a condition that can run in families. It affects the genes inside the cells in the body, causing the gene to give incorrect instructions to the cell, and not work properly. This gene change is often called a variant or mutation.
Diagnosing LS is usually by genetic testing. Those diagnosed with LS are entitled to earlier screening, which is also completed more frequently.
Risk reducing treatments such as taking aspirin, H. Pylori testing and treatment, which is a stomach bacterium that can increase the risk of stomach cancer, and surgery.8
• Collaboration
It is the responsibility of local systems to organise their cancer workstreams and partnerships to work to national guidance and advice (outlined by NICE, NHS and governmental agendas) and ensuring these are represented and in place at a local neighbourhood level. These are often made up of Integrated Care Board (ICB) (including hospitals, primary care networks), local authorities and quality assurance organisations.
Many collaborative meetings also include patient representatives, as it is understood and recognised how important the patient perspective and experience are, to inform partnerships, and ensure services are delivered with and not to those that use them.
The voluntary sector is also key, with many organisations and charities offering vital support groups and other opportunities to those affected by cancer; this includes not just the patient themselves but the wider family, recognising the wider impact cancer has for many.
Working together in partnership supports patient services being the right ones, delivered in the right places, increasing accessibility and reducing inequalities.
 Latest Derbyshire Data
Latest Derbyshire Data
Trend Data
Prevalence Maps of Derbyshire
The maps below illustrate various geographies for Derbyshire. LSOAs and MSOAs are geographical divisions used for statistical purposes, allowing for more detailed analysis of local data. In these maps, you can explore various health indicators and data for Derbyshire, providing valuable insights into the area’s health and wellbeing.
Wards Data Not Available
Data for this geography is not yet available. Please check back later.
Districts Data Not Available
Data for this geography is not yet available. Please check back later.
 |
In the top right of the map, you’ll find the ‘Layer Control’ icon. This is an easy way to customise what you see on the map visualisation. Click the ‘Layer Control’ to choose which information is displayed on the map. Pick the indicator that interests you the most, and the map will transform accordingly. |
Slope Index
This chart illustrates the differences in health and lifestyle factors across areas in Derbyshire, from the most deprived (decile 1, red) to the least deprived (decile 10, green). As you move from left to right on the chart (from more deprived to less deprived areas), the line shows whether these factors are becoming more or less common. Essentially, it’s a way to see how living in wealthier or poorer areas affects the prevalence of these factors.
 Further Analysis & Assessments
Further Analysis & Assessments
Derbyshire Joint Strategic Needs Assessment (JSNA) involves a thorough examination of a specific health problem, exploring its causes, consequences, and underlying factors. It combines various data sources, collaboration with stakeholders, and rigorous analysis to generate insights for evidence-informed interventions and policy changes.
 More Information & Resources
More Information & Resources
Here is a list of useful resources and information with regard to bowel cancer. These materials are meant to provide individuals, healthcare professionals, and communities with the knowledge and tools they need as part of efforts to address bowel cancer as a population health topic.
Contributors
Stacey Speed, Advanced Public Health Practitioner and Charlotte Reece, Advanced Public Health Practitioner